By: An RFC Patient
Let’s start with a general disclaimer: the below blog is my personal journey with IVF, and is not meant as medical advice, etc. I also am not a doctor or anyone in the field—this is just my experience with IVF as a PCOS patient. I will be getting into some nitty-gritty below that is more PCOS-specific. Now, let’s get to the good stuff.

What is IVF?
IVF stands for In-Vitro Fertilization. A simplified explanation is: the patient takes meds to mature eggs, you then have a procedure to remove the eggs from the ovaries, and sperm are either mixed or injected into the eggs, hopefully resulting in embryos. The last step is the transfer of one (or multiple) embryos back into the uterus, either directly after the retrieval or months later via a FET (frozen embryo transfer).
Worth noting, IVF is not a one-size-fits-all. You’ll want to discuss all your health issues (including PCOS) with your infertility specialist so they can custom tailor your protocol and medications.
PCOS & IVF Quick Notes
Since I went into IVF with no knowledge and research (why? palm-to-forehead smack), I thought I’d spare you and add these quick notes.
- PCOS tends to slow the maturation of eggs (so for me, the longer IVF protocol made a world of difference).
- PCOS patients can have a higher rate of OHSS (Ovarian Hyper Stimulation Syndrome) after egg retrieval.
- My specialist’s protocol included a steroid to aid with decreasing inflammation and neutralizing reactions to the implanted embryo. I found this very beneficial.
1. Infertility Pre-Testing
During your infertility journey, you’ll probably undergo quite a few diagnostic tests. It’s important to know what’s happening in your body before you invest both time, money, and hope into your infertility treatments. This is especially important for PCOS patients as we are prone to cysts and endometriosis.
- Ultrasound and blood work. I was checked for ovarian cysts (beyond the PCOS cluster). A large ovarian cyst was found, one that I had no clue existed.
- Hysterosalpingogram (HSG) to check for fallopian tube obstructions (not required for IVF, but was for general infertility). I found out that one tube was completely blocked. Again, I had no idea. This further pushed us towards IVF as my roads were blocked.
- Hysteroscopy, which is a more invasive ultrasound of the uterus. Oh, guess what, they found I had fibroids, which can prevent implantation or cause miscarriage.

Let’s not forget that endometriosis tends to go hand-in-hand with PCOS, so I also had surgery to remove possible endometriosis. This was more an exploratory surgery, and the doctor (my ob), who assumed it was a light case of endometriosis, told me it was one of the worst he’s seen.
I had PCOS, Endometriosis, fibroids, an ovarian cyst, and blocked tubes—no wonder I went years struggling to get pregnant! And no, I had no symptoms of the cyst, the blocked tubes, or fibroids!
Before proceeding with IVF, I had to address all these issues. But once my engine was clean, I was ready to move forward and thankful for all the diagnostics.

2. Choosing the Right Doctor
Before I get down to my IVF specifics, let’s talk about reproductive endocrinologists and finding the best fit for you. You’ll want to look at the doctor, their success rates, their ratings, and their staff. You’re putting a lot of time, money, and trust into this doctor, so make sure you are one-hundred percent comfortable with them.
I am a patient, a repeat patient, of Dr. Lin. If I could describe him in one word, it would be chill. This may seem like an odd description, but I have anxiety, so to find a doctor who’s relaxed, friendly, optimistic—and chill is a big deal for me. I had extreme anxiety leading up to my initial IVF consultation, and I almost felt like a failing student going to see a strict professor. But Dr. Lin was friendly, not rushed, and his focus was on us, talking us through everything while taking his time to explain and answer questions. Maybe personable is a better word to describe him. I didn’t feel like a number, which, unfortunately, I feel like quite often. And let’s not forget the staff! My IVF coordinator at RFC has been an IVF coordinator/nurse for twenty years! Twenty years!
Trust, patient/doctor relationship, and the overall tone of the office, and their passion for helping you are pretty important to your success. Find a specialist that meshes with your style and your needs. This is a big investment in all aspects, so you want the deck stacked in your favor.
3. IVF Protocol
I went into IVF blindly. I barely knew anything about it and assumed it was a one-size-fits-all. IVF protocol? What’s that? My first protocol was unsuccessful. But before I continue, remember that all bodies are different and will respond to medications differently. When I went in for my initial testing, my PCOS symptoms were very controlled. At that point, I had very, very mild PCOS (after working for years to get it under control).
Due to my lack of PCOS symptoms, I was put on an ‘Antagonist’ protocol. This was an 8-day protocol that resulted in very few embryos, only one of which made it to the blastocyst stage. Unfortunately, this embryo did not make it past implantation. I’m not sure why this protocol didn’t work for me, but like I said, all bodies react differently.
After the first IVF protocol, my PCOS symptoms went crazy! We’re talking from zero to sixty overnight. So my second protocol was more in line with severe PCOS. I was put on a ‘Micro Flare’ protocol, and holy-moly! This was a 9-day protocol that resulted in almost triple the number of mature eggs. I do believe that extra day helped mature the follicles since PCOS tends to delay maturity.
The Micro Flare protocol used the same stim meds as the Antagonist protocol, as well as Lupron (Leuprolide). For me, this made all the difference. I don’t know what exactly it did, only that my mature eggs tripled in count from the first protocol.
4. Your Follicles and PCOS
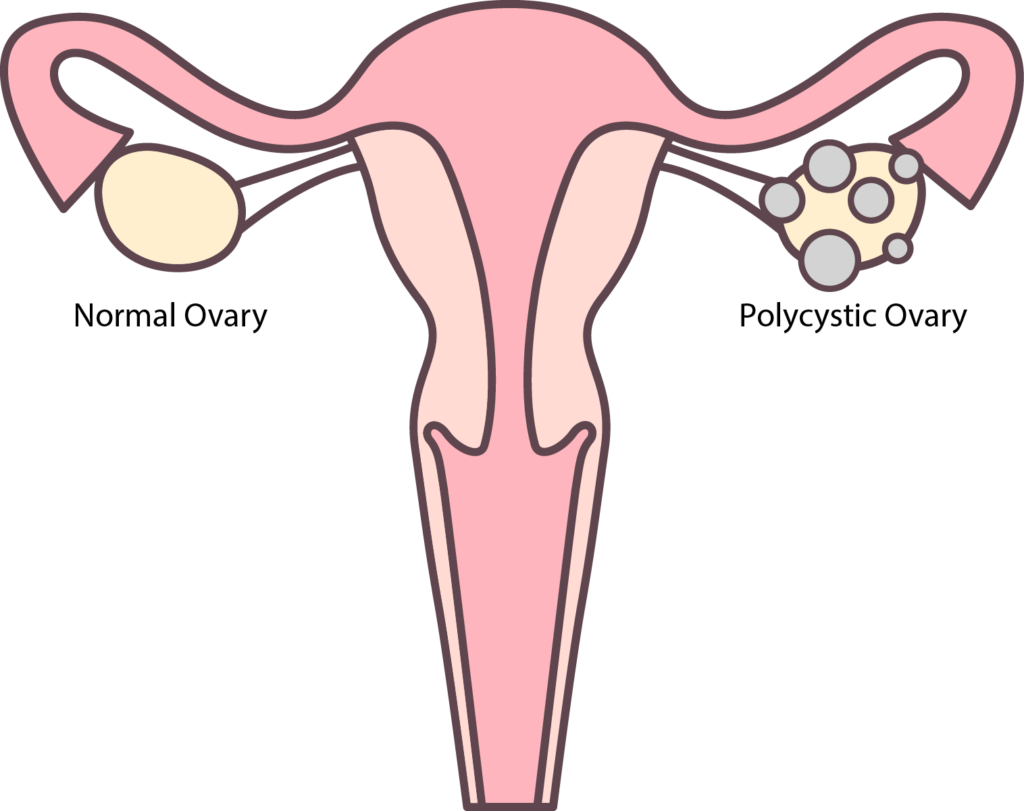
Another joy of PCOS is the ton of immature and stubborn follicles already filling your ovaries. Your specialist will probably get excited seeing all those little ones until you remind them that you have PCOS and those stubborn follicles will not grow, and if they do, they will probably not be viable.
For IVF, they like to see all the follicles growing to be the same size, or at least close in size, and will adjust your meds to try and grow these follicles. Well, if you’re like me, you’ll have a few lead follicles, then a bunch of non-growers. If your doctor is not well versed with PCOS, then they may try to push your meds to grow those little follicles, which risks the health of your lead follicles. It is important to understand the correlation between PCOS and follicle growth and maturation.
5. Fresh Transfer vs. Frozen Transfer with PCOS
Now, you’ve got some eggs on their way to becoming embryos and it’s time to decide if you want a fresh transfer after retrieval or to freeze the embryos for a later frozen transfer (FET). I read a lot of papers and studies about this specifically for PCOS patients. These studies hinted that because PCOS eggs mature slower and tend to need some extra TLC that there were benefits to doing a two or 3-day transfer and letting them develop within the uterus, as opposed to maturing in an IVF culture dish until day five or six. After going back and forth, and back and forth, I came to the decision that I wanted a 3-day transfer.
The preference I believe most doctors have is to wait until day five or six to see if the embryo makes it to the blastocyst stage, which is a good sign that the embryo is strong. The problem is that some, heck, many embryos don’t make it to day five. This is where you hear stories of how someone has twenty eggs retrieved, but by the end of the week, there are only three embryos remaining—survival of the fittest.
Well, after all that worry and research, after all the talks with Dr. Lin on the best strategy for my PCOS eggs, I failed to think about the fact that because of my PCOS and the number of follicles this protocol produced that I was at an increased risk for OHSS (Ovarian Hyper Stimulation Syndrome) and if you get this then a fresh transfer is typically out of the question. Dr. Lin had warned me of this, but I took it in stride because I didn’t know any better. I was young—I would be fine. Guess what; I got it. So, instead of moving forward with the 3-day transfer and risking my and the health of the embryos, I decided to wait a few months and do a FET protocol.
I did, however, still opt to freeze some eggs at 3-day, versus the standard five-day period and transfer those 3-day embryos at a later date.
6. PCOS and OHSS (Ovarian Hyper Stimulation Syndrome)
There are many known risks and warnings with IVF, but one I hadn’t heard about that is especially relevant for patients with PCOS is Ovarian Hyper Stimulation Syndrome. So here’s what happens after an IVF egg retrieval procedure: eggs are retrieved, and the now-empty follicles fill with liquid—the more follicles, the more liquid. This happens anywhere from immediately after the procedure to weeks later.
OHSS causes you to swell and bloat and can make breathing difficult. My mild OHSS subsided after about ten days. I had to sip Gatorade and Pedialyte constantly to help absorb the excess liquid and contain the bloating.
PCOS patients are more at risk, so it’s worth searching this term and looking into symptoms, risks, and how to treat if you get it.
7. Steroids Before Transfer
I wouldn’t normally add this, but I feel it’s relevant to PCOS patients. Before my FET, I was prescribed Prednisolone (aka Prednisone), a steroid you take orally. So, I went off to research and found the results overwhelmingly positive, with some articles even calling the steroid a ‘wonder fertility drug’. The steroid is used to decrease inflammation (which PCOS is all about) and help neutralize reactions against the foreign embryo to increase the chance of implantation. This is definitely something to add to your research list and talk to your doctor about.
IVF Final Thoughts
Here are some of my personal final thoughts, things I wish I would have known or thought more about when going through it the first time.
- PCOS eggs need a little more time to mature and the focus should be on quality, not quantity.
- The stim meds can trigger your PCOS symptoms. I went from none to overwhelming symptoms right after.
- PCOS patients are at a higher risk for OHSS, make sure to prep just in case.
Hope this was helpful!



