My PCOS diagnosis
I was first diagnosed with polycystic ovary syndrome (PCOS) when I was around 16 to 18 years old. I was just going in for a routine check-up with my gynecologist. I was having irregular periods so I got an ultrasound, and that’s when I found out I had PCOS.
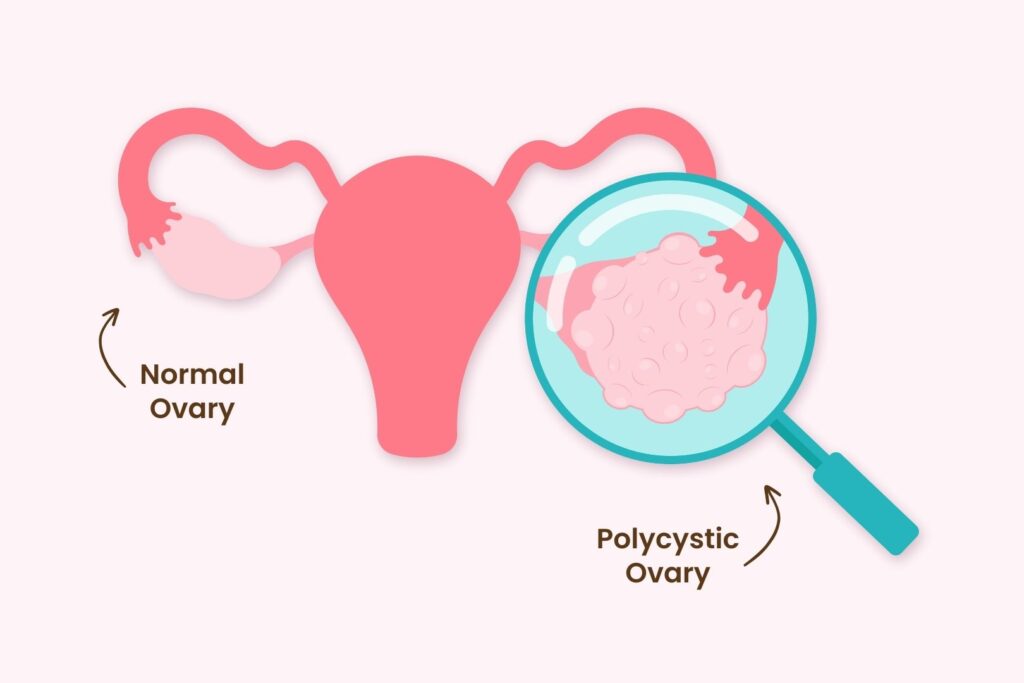
Polycystic ovary syndrome is a hormonal disorder where the ovaries produce abnormal amounts of androgen, male sex hormones. The imbalances in hormones lead to enlarged ovaries, causing symptoms like irregular periods and lack of ovulation, making it difficult to become pregnant.
My doctor told me that because of my diagnosis, I would have difficulties having kids later on. But I was so young at the time and felt so far away from having children, I wasn’t too worried. Of course, it was disheartening news, but it just didn’t sink in then.
It wasn’t until I got married in my early 20s and wanted to start having kids, that I really felt the impact of having PCOS.
I wasn’t having regular periods and I wasn’t getting pregnant. That’s when I started getting concerned about whether or not I would be able to get pregnant. I was struggling and became very discouraged at that point.
PCOS then vs. now
PCOS was treated very differently 30+ years ago. If you weren’t able to ovulate, there really wasn’t much that could be done about it.
Back then, PCOS medications were used to help you ovulate, but there weren’t many factors you could control or information on how and when to use them. There were a lot of uncontrollable factors.

When I started taking medications for PCOS, I had a lot of ups and downs with my medications either not working at all or working too much. I started with oral medications and I just didn’t respond to them. Then, I started doing injectables, and those worked too well to the point where I had ovarian hyperstimulation, which is when the ovaries swell and become painful due to excess hormones. My estrogen levels shot way up and I produced a lot of eggs.
Today, monitoring techniques are better and we can get more information to understand the factors of PCOS. There are also better ways now to minimize ovarian hyperstimulation when inducing ovulation. Even with ovarian hyperstimulation today, we can retrieve the eggs and freeze them for future family plans. 30 years ago, freezing your eggs was not common and the risks of doing it were too high.
My transition from OBGYN into fertility
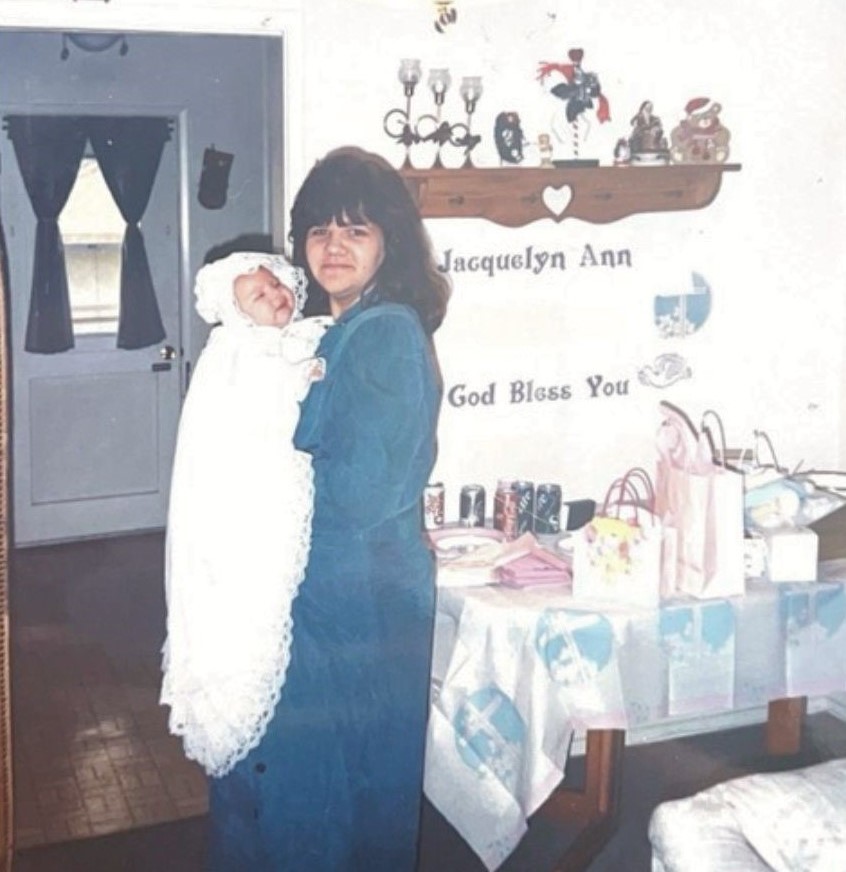
Once we got my medications just right, I had eggs, and I was ovulating, so I convinced my nurse practitioner to do intrauterine insemination (IUI). And, to my luck, it worked! I was pregnant and was able to have a beautiful daughter.
At that time, I was working in obstetrics and gynecology. My experience with PCOS and fertility challenges is what inspired me to switch to the fertility field.
I was working with OBGYN physicians and nurse practitioners. We had a reproductive endocrinologist and infertility specialist come in once a month for our OB patients. Initially, I was only involved with fertility treatments like inseminations and monitoring. But the more I got involved, and in conjunction with my own fertility experiences, the more I knew I wanted to switch fields.
That’s actually when I met Dr. Lin; he was one of the REI doctors who came in once a month. I’ve been working with him ever since.
Leaving my mark
Working in obstetrics and gynecology, you see a lot of patients on a day to day. The support I could give to OB patients felt limited. In fertility, I felt like I could be more involved with patients’ journeys since fertility patients have more follow-up appointments and their treatments are more time-sensitive. Because of this, I felt like I was able to have more face-to-face interaction with them and develop a deeper connection.
Transitioning into the fertility field was a natural progression for me. My own fertility experience gave me a great sense of empathy and I wanted to be more involved with patient education and more importantly, supporting individuals and couples struggling with fertility.





When you’re going through these challenges, it’s extremely isolating. Infertility, especially back then, is seen as a taboo and it’s not something most people feel comfortable openly talking about.
So, the mark I want to leave is my support. Working in fertility clinics, I can give patients support and a shoulder to lean on when they feel like they can’t open up to anyone outside of the clinic.
Fertility challenges are difficult to share with your friends and family, but I want our patients to feel like they can share with their fertility team. I want to be able to answer our patients’ questions, listen to their concerns, and just be on their side because everyone needs someone. No one should go through their fertility journey alone and I want our patients to know that they don’t have to.




