From the Storm to the Rainbow
By: S.S. (Actual patient of Fertility Specialist, Dr. Lin, of Reproductive Fertility Center in Irvine, California)
Let’s start with the basics before I dive into my journey with PCOS.
What is PCOS?
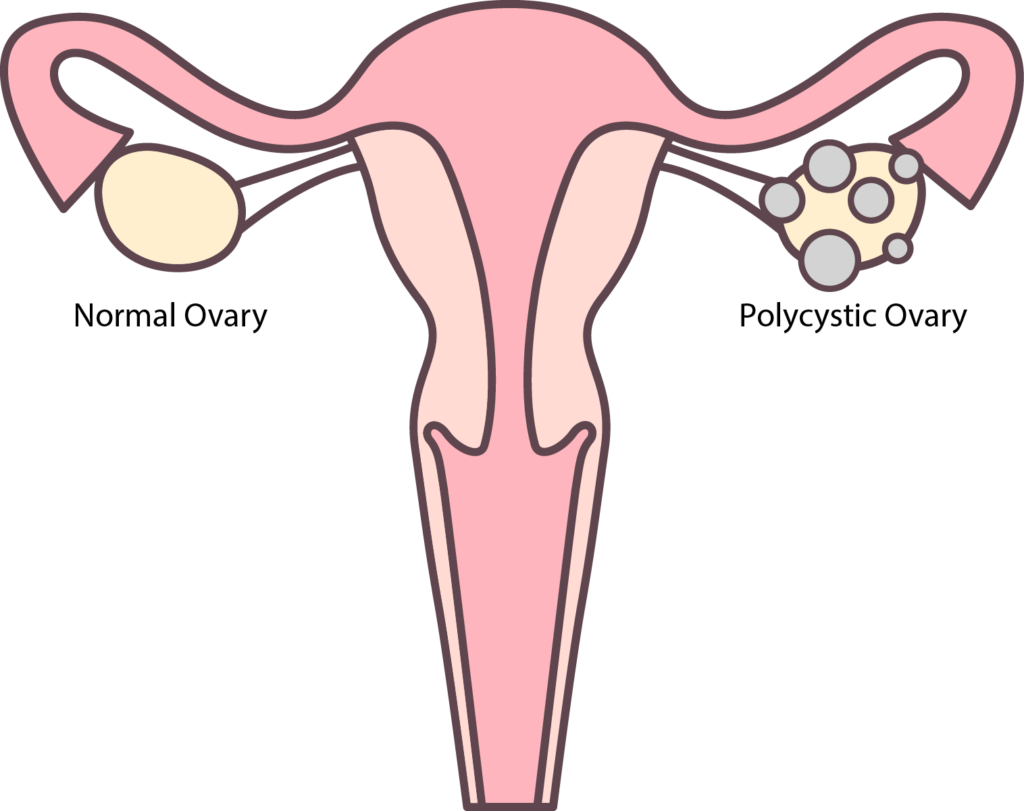
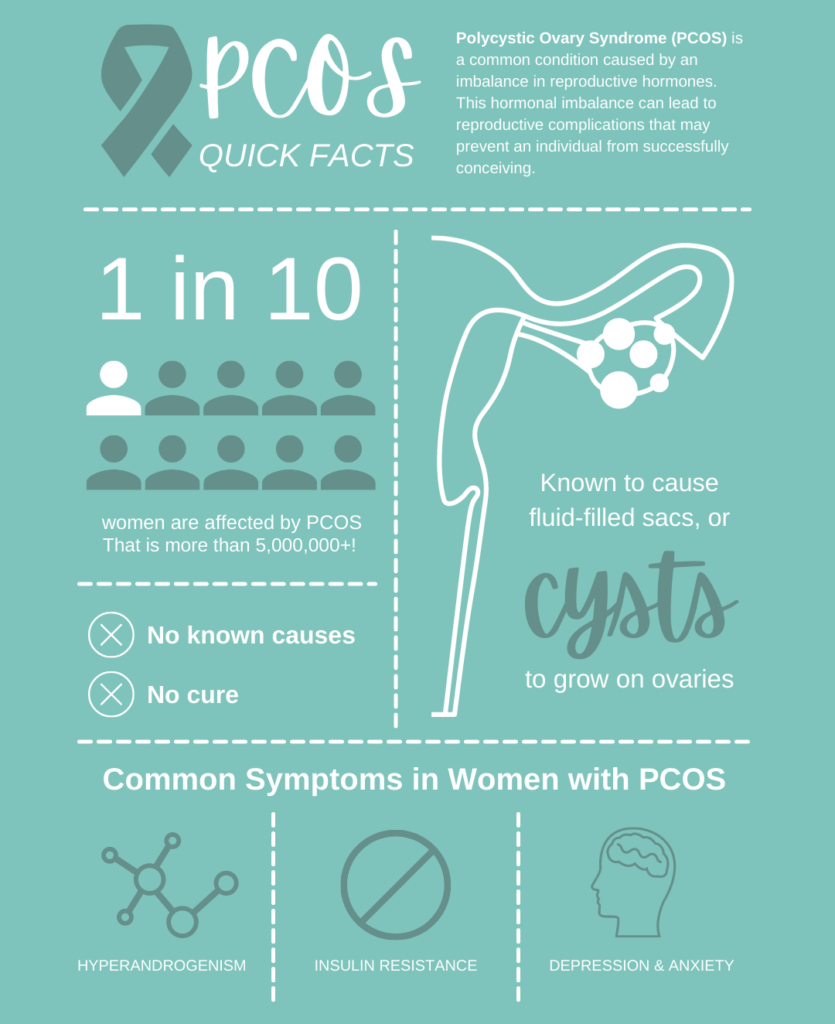
For those landing here randomly, curious about what PCOS is, let me break it down for you. PCOS stands for polycystic ovary syndrome—something I was diagnosed with in my teens! PCOS is an endocrine disorder in persons with ovaries, and the CDC estimates that there are over five million cases of PCOS in the United States alone!
And guess what—it’s also one of the most common causes of infertility.
My PCOS Symptoms
PCOS symptoms vary from patient to patient, both in the actual symptoms and their severity. My first symptoms were:
- weight gain, especially around the stomach (cushioning those cystic ovaries)
- cystic acne, covering every inch of my face
- polycystic ovaries
- hypoglycemia
- anxiety
- depression
- infertility
- craving sugar like it was a drug (A dozen donuts? Make it two!)
Other common PCOS symptoms:
- irregular period
- excess hair growth on the body
- and ironically, hair loss or balding
- tubular breasts
- darkening of skin
- headaches
My PCOS Diagnosis
I got lucky in the diagnosis department. I was diagnosed by a doctor right away. I assumed this was standard practice until I joined the PCOS community (by the way, September is PCOS awareness month!). I was shocked that women spent years with these symptoms and: a) assumed it was just a part of aging, and/or, b) couldn’t get a doctor to take their symptoms seriously.
PCOS symptoms are often brushed aside, especially acne, weight gain, fatigue, inability to lose weight, sugar cravings, mood swings, depression, and anxiety. If I had a dime every time I heard someone (doctors included) say, “It’s part of getting older,” or my favorite, “Just lose some weight.”
You know your body. I knew that when I went to bed with crystal clear skin, as I had every night before that, and woke up with—no joke—instant cystic acne, that something was wrong. Now, looking back at my childhood and early teens, I see that PCOS was always there. I’ve craved sugar for as long as I can remember, think about going to a birthday party just for the cake.
You must fight for your health! Especially with PCOS! Why? Drum roll, please—there is NO cure for PCOS! Doctors can’t prescribe you a pill to take it away, and there is no surgery or procedure to rid you of it.
I had to force myself to fix my relationship with food, increase my physical activity, proactively address my symptoms, and try to push through them—on top of everything else that life was throwing at me.
My PCOS Attack Plan
Step one was to research PCOS. I read all the health articles and all the personal journeys of those before me. This gave me insight into PCOS as a whole and how others were navigating their symptoms.
Step two was to start on a supplement plan. I won’t go into specifics here, but I encourage you to do some searches on PCOS supplements. Different supplements target different PCOS symptoms.

Step three was to overhaul my diet. If you have PCOS, then chances are you crave sugar like an addict—this might be an understatement! Your body has no idea what to do with insulin. PCOS has crossed those wires and blocked that regulation, so we require more sugar. Let’s be honest, I could eat sugar-based foods every meal of the day. I have zero interest in anything salty—nada. But more sugar means more inflammation. So I took inventory of all the sugar I was actually eating in a day and knew I was out of control. Thus, I started ditching processed sugars and desserts, bread was next (although I would have some sourdough now and then), and milk followed.

Next, I began swapping in healthier foods. I added more fish, more salads, more fruit, and more nuts to my daily meals. When I needed a snack, I’d opt for carrots instead of chips. When I needed sugar, I’d opt for grapes, strawberries, or dark chocolate.
Please note that this was not an overnight change. I had to wean myself off of the sugar, processed foods, snack foods, chips, and fast food. By weaning and adding, I was able to make a lifestyle change—not just a diet change.
Step four was to get more physical. The gym was a no-go for me, so I stuck to walking. Never underestimate the power of walking! Not only was walking good for my cardiovascular health, but the sunshine and fresh air helped my depression and anxiety.
I added weights into this to reap more rewards. Muscle building is great for PCOS and helps with weight loss.
And guess what! After two years of self-care, I was acne-free, had lost twenty pounds, my depression turned to just a one-week-out-of-the-month event, and my sugar cravings were almost gone. (I actually said no to donuts, and it didn’t kill me inside.)
Yah—I was healed—I’ll surely get pregnant now!

PCOS Infertility
Welp, as I said before, there is no cure for PCOS, and while the majority of my symptoms had cleared and my cycle was regular—I still could not conceive.
This led to a series of tests, where it was discovered I also had endometriosis. Subsequently, while looking into this, I found a high correlation between women who had PCOS and endometriosis. Optimistically, I hoped that by having surgery to remove the endometriosis, I would be able to conceive. Nope.
So now started the PCOS ovulation protocol, which typically starts with Letrozole (Femara), a drug similar to Clomid to induce ovulation. Letrozole apparently has higher success rates for PCOS patients. I was optimistic again, started the drug, went through more than a few cycles. Nope.

I was sad. Depression crept up, eating healthy went rogue, exercising turned into laying in bed. The stress, the disappointment, the drugs were fast-tracking my PCOS symptoms, not only the physical ones like cystic acne and weight gain but depression and anxiety as well. Take the disappointment of infertility, mix it with a double dose of depression, and bam—you’ve got yourself into a crazy mental storm.
I’d done everything I could to conceive, but it wasn’t happening.
This was when I decided to take my fertility future out of my OB’s hands and into a fertility specialist’s—Dr. Lin of Reproductive Fertility Center, in Irvine. I’m an actual patient, a recurring patient, actually. If you’re there, you just might see me!
Getting pregnant with PCOS
Once with Dr. Lin, our options moving forward were IUI or IVF. And my personal decision was to go straight with IVF. Why? As mentioned above, I’d spent far too long in a PCOS cloud of depression and anxiety. We’re talking four years of trying to conceive. An IUI would set us back further (if it didn’t work), and it was common to have multiple IUIs.
Were we willing to wait through more months of maybes? Nope.
Were we up for that roller coaster of emotion from hope to that nosedive of despair if it didn’t work? Nope.
Did we want to jump to the surest thing (for us personally)? Yes!
Was I willing to go through the medications and embryo retrieval to conceive? Yes.
PCOS & IVF (In-Vitro Fertilization)
Let me tell you—I wish I could go back in time to convince myself to move forward with a fertility specialist sooner and not be so worried about IVF. It really wasn’t anything like what I’d imagined, and I wasted countless hours of anxiety about it.
I know the first thing that came to our mind, even before medication and all that, was the cost. IVF is expensive! But so were constant doctor appointments, ultrasounds, medications, blood draws over those four years—and possible future. We were also incredibly lucky that our insurance covered a portion of the cost. We agonized over our out-of-pocket portion (all of which went on a credit card), then spent a few years paying it off. Now, it’s nothing more than a fleeting thought.
After you’ve crossed the financial hurdle, it’s time to talk about IVF protocol. IVF is not a one-size-fits-all. There are standard protocols, but they will get tweaked for your needs. Tell your fertility doctor that you have PCOS! This is very important! They will adjust your protocol accordingly and monitor your response to the drugs. Don’t assume the doctor will see your polycystic ovaries during an ultrasound and label you as PCOS. Remember, be your own advocate.
Here’s a pretty accurate transcription from my first visit with Dr. Lin:
{Sits silently for five minutes because she’s too nervous.}
Then randomly blurts out, “I have PCOS and endometriosis.”
One year later, I sent his office a birth announcement.
I’ll save the exact details of my protocol, meds, my IVF adventure, etc., for another time as this blog is turning into a novel.



